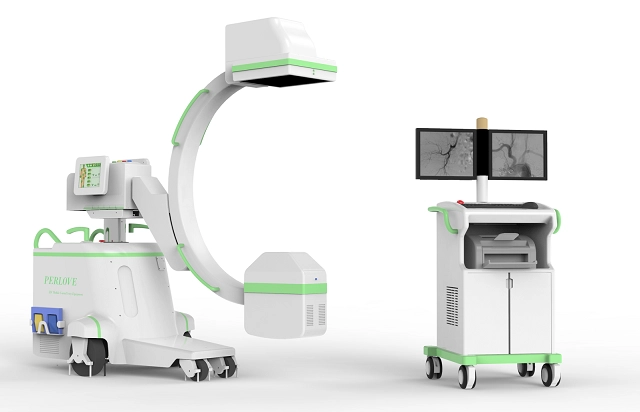
Endoscopic retrograde cholangiopancreatography, or ERCP, is a procedure to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas. Check our latest case report of #ERCP assisted by High Frequency Mobile Digital C-arm System #PLX7100A #Perlove

What is ERCP?
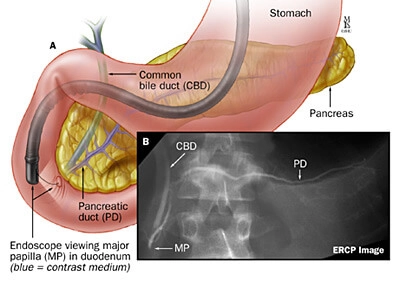
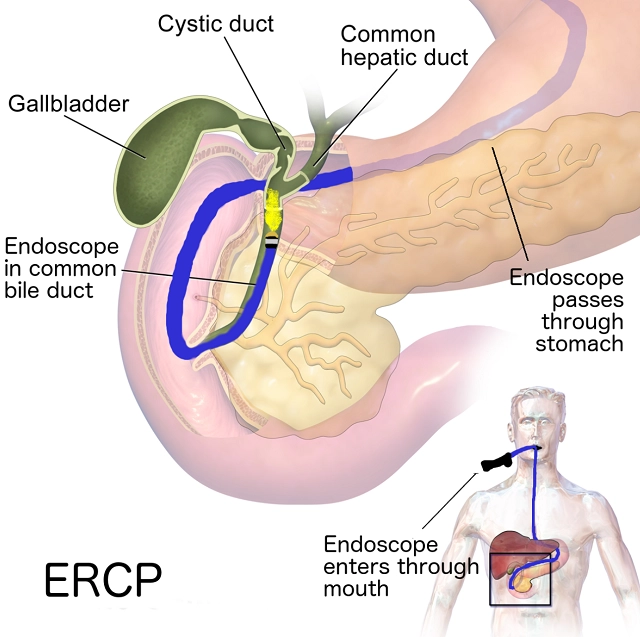
Endoscopic retrograde cholangiopancreatography procedure (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems.
Copyright: Johns Hopkins Medicine
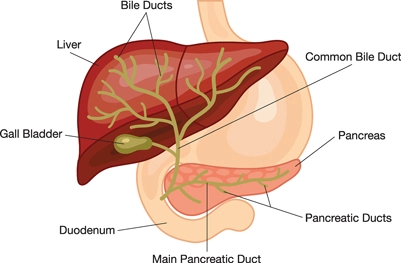
What are the bile and pancreatic ducts?
Bile ducts are tubes that carry bile from liver to gallbladder and duodenum. Your pancreatic ducts are tubes that carry pancreatic juice from your pancreas to your duodenum. Small pancreatic ducts empty into the main pancreatic duct. Your common bile duct and main pancreatic duct join before emptying into your duodenum.
Why do doctors perform ERCP?
Doctors perform ERCP when your bile or pancreatic ducts have become narrowed or blocked because of gallstones, infection, tumors or cancers of the bile ducts or pancreatic ducts…
Case report
Endoscopic retrograde cholangiopancreatography procedure
Introduction
In January 6, 2021, a case of Endoscopic retrograde cholangiopancreatography procedure (ERCP) was performed in Jiangbei International hospital affiliated to Nanjing Drum Hospital China.
Clinical history
Female, 82 years old, confirmed with cholecystitis and common bile duct (CBD) stones through magnetic resonance cholangiopancreatography (MRCP) 4 month ago. Patient has recovered in good condition after first ERCP. Yet recently patient has experienced abdominal pain again. CT scanner shows that:
(1) local extension of intrahepatic bile ducts and pancreatic duct, CBD has a more distinctive extension than previous diagnosis;
(2) CBD stone with sign of inflammation;
(3) calcification spotted under Glisson’s capsule of right liver lobe;
(4) multiple tiny lymph nodes spotted on liver;
(5) possible occurrence of spleen calcification;
(6) thickening of right adrenal gland;
(7) calcified nodules were found on right lung.
Surgery
(1) Esophagogastroduodenoscopy (Olympus CV290) was inserted into patient’s mouth after successful anesthetization, it travels through esophagus into stomach, arrives at duodenum.
(2) When the endoscope arrives at middle part of duodenum where major papilla is located, air is insufflated to distend the duodenum and allow visualization of this particular part. Then a guide line and a catheter are inserted through the opening of the papilla to gain access to the CBD.
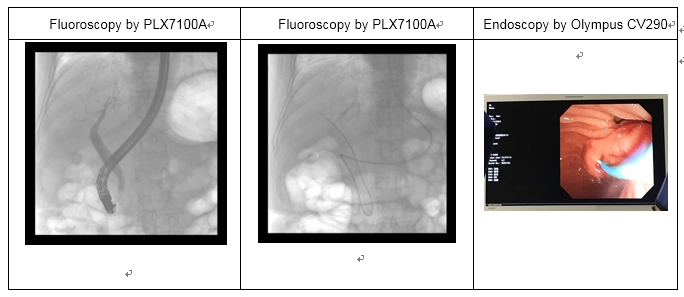
(3) Contrast agent are subsequently injected into the bile duct allowing surgeon to inspect the biliary tree and locate the stone through fluoroscopy (using PLX7100A, Perlove Medical).
(4) The stone are removed by pulling it out the duct and into the small bowel using a balloon to sweep and clean the duct. It then can be discharged out the body through the gastrointestinal tract.
(5) Radiography (using PLX7100A Perlove Medical) are applied to assess the surgical outcome. Then remove the endoscope, sew up the wound and end the surgery.
Outcome and image analysis
The surgery are successful and stone are removed outside the body. With clean dynamic fluoroscopy image demonstrated during the surgery, High Frequency Mobile Digital C-arm System PLX7100A was highly spoke of by surgeons. The sharp image perfectly revealed patient’s biliary and pancreatic structure as well as located the stone, which proved PLX7100A are as remarkable as its competitors.
-
Perlove Medical at ECR 2026: Showcasing Cutting-Edge Imaging Solutions in Vienna
Read More » -
🌍 Elevating Global Healthcare | WHX Dubai 2026 Successfully Concluded
Read More » -
Join Us at ARAB HEALTH 2026 | See You in Dubai
Read More » -
Surgical Robots Take the Stage in the “Battle to Protect the Spine”
Read More » -
Application of 3D C-arm Imaging in Radiofrequency Ablation Treatment of Trigeminal Neuralgia
Read More » -
Correcting Limb Length Discrepancy | 3D C-arm Assisted Epiphysiodesis in Pediatric and Adolescent Patients
Read More »





